The medical world can be confusing from a patients perspective. Diseases that sound related might not be and diseases that sound totally different might be. In the case of psoriasis vs psoriatic arthritis, it’s not really any simpler. Based on the names of the conditions, you might assume they’re somehow related, and that’s true. However, there are also considerable differences to set them apart.
If you or a loved one have been diagnosed with either condition, you’re likely wondering about the connection between these two conditions. In today’s blog we’ll break down exactly how they are related, and how they aren’t, to help you move forward with a practical understanding of the two conditions.
What connects psoriasis and psoriatic arthritis?
At the core of all symptoms of both psoriasis and psoriatic arthritis is inflammation. This inflammation is caused by the immune system attacking cells that it shouldn’t and wouldn’t normally. Since both of these conditions are caused by problems with the immune system, around one in three people diagnosed with psoriasis will also be diagnosed with psoriatic arthritis.
It isn’t necessarily clear that psoriasis is a cause for psoriatic arthritis but it is considered to be the single greatest risk factor as it indicated an already compromised immune system. Unfortunately, doctor’s aren’t usually able to determine who might develop psoriatic arthritis after psoriasis, but people with very severe psoriasis may be at a higher risk.
Another link between psoriasis and psoriatic arthritis seems to be genetic, although researchers have not pinned down the link exactly. Around 40% of people with psoriatic arthritis have relatives with psoriasis, indicating some kind of further connection between the conditions.
What sets psoriasis and psoriatic arthritis apart?
It’s clear that there is some kind of connection between psoriasis and psoriatic arthritis even if researchers haven’t completely defined it. However, there are some boundaries that this connection does not extend to. The most noticeable difference is that there is no connection whatsoever between the location of psoriasis patches on skin and psoriatic arthritis in the joints. This means that you could have lesions on the skin around your knees but absolutely no impaired function moving or bending it, even if you have both psoriasis and psoriatic arthritis.
Another major difference between psoriasis and psoriatic arthritis is the lasting impact on affected areas. Once psoriasis patches go away it’s as if they were never there, and the skin can heal can completely. Unfortunately, if not treated properly and in time, psoriatic arthritis can cause permanent damage to joints.
The bottom line:
The bottom line is that psoriasis and psoriatic arthritis are two separate conditions but share many links. One of the final links they share is actionable next steps you may be able to take if you’ve been diagnosed with either.
Obviously, the most important thing you can do is work with your doctor to find the right medication and treat the condition, but there are numerous lifestyle changes capable of making a big impact, regardless of which condition you’re treating.
- Control stress: Oftentimes flare-ups in inflammation leading to symptoms can be linked to increased stress. Controlling stress is easier said than done, but by identifying triggers you can work to achieve or more stress-free life. You may also find that speaking with someone you trust of a therapist can help with this.
- Maintain a healthy weight: Being overweight plays more of a role in worsening psoriatic arthritis than psoriasis, as it puts additional stress on joints. This stress can cause or worsen inflammation. If you’re not sure where to start with losing weight you can speak with your doctor or a dietician.
- Eat healthier: Losing weight isn’t the only potential benefit of eating healthier. Certain foods are linked to increasing or decreasing inflammation. By managing your intake of these foods you can better control your inflammation. Click here for a list of some foods that can increase and decrease inflammation.
- Stop smoking: Smoking has numerous negative effects on your health but some studies have shown it can also reduce the effectiveness of treatment.
- Remain physically active: Aside from the potential of losing weight, regular exercise, even if it’s as simple as taking a walk, can help joints from getting stiff. One of the best low-impact exercises for people with psoriatic arthritis is swimming, as it reduces the risk of triggering a flare-up through overuse but provides the benefits of rigorous physical activity.
Here are some other articles we think you might enjoy:
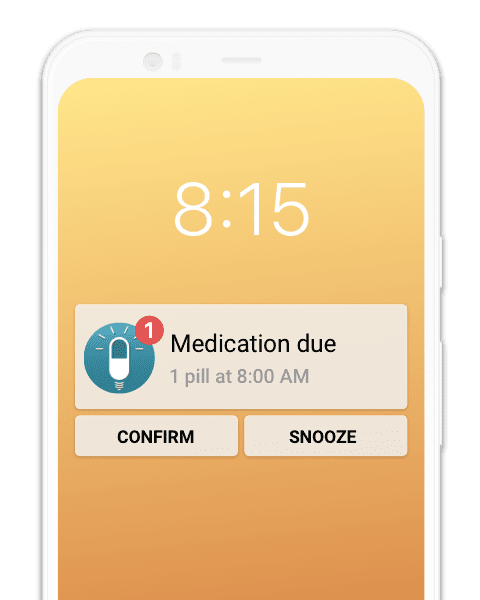
3 Innovative Apps Making Life with Psoriasis Easier
Anti-Inflammatory Foods for Arthritis and Psoriasis Diseases